Intern Ultrasound of the Month: DVT Diagnosed at the Bedside
The Case
75-year-old female with PMH including bladder cancer requiring indwelling foley and nephrostomy tube placement who presented to the ED for suprapubic pain and decreased urine output.
On arrival, she was mildly tachycardic with low normal blood pressure and was noted to be uncomfortable-appearing. Exam was significant for suprapubic tenderness, along with right lower extremity edema.
Point-of-care ultrasound was used to assess for DVT and urinary obstruction. Around this time the patient became hypotensive, so a RUSH exam was performed as well to assess for etiology of hypotension. Significant findings were noted when evaluating the RLE as shown in the following images:
Noncompressible proximal femoral vein w/ echogenic clot
Saphenofemoral junction - greater saphenous vein branches off medially/superficially
No flow seen on Color Doppler
Near bifurcation of deep femoral vein. Still noncompressible
Noncompressible popliteal vein sitting on top of popliteal artery
POCUS findings: non-compressible femoral vein with echogenic clot visualized within the lumen — consistent with DVT.
Not shown here but cardiac POCUS showed grossly normal function without signs of right heart strain or effusion, there was no significant urinary retention or signs of hydronephrosis, and RUSH exam was otherwise unremarkable.
Case continued: BP responded to IV fluids. She was preemptively started on heparin and taken to CT for a CT PE study + abdomen/pelvis, which showed extensive bilateral PEs but no acute abdominal process. Similar to POCUS findings, there was no evidence of right heart strain on imaging or labs. She remained relatively stable, was treated for UTI, and admitted to the hospital for further management. She had no major complications, was transitioned to oral DOAC, and discharged to a nursing facility.
Deep Venous Thrombosis
Background/Review [1]
DVT: thrombus formation in a large vein of the extremity
90% are in the lower extremity
Of patients with DVT, 40% have PE
Of patients with PE, 70% have DVT
Risk factors: age >60 years, cancer, CVC insertion, genetic causes of hypercoagulability, history of DVT, immobilization, obesity, pregnancy, smoking, trauma or recent surgery, OCPs or hormone replacement therapy
Upper extremity is typically related to venous catheterization
Management depends on patient stability
Heparin vs DOAC
Mechanical thrombectomy if extensive clot burden
Use risk stratification scores (Hestia, PESI)
Complications include:
Without treatment can progress to PE
Post-thrombotic syndrome
Venous gangrene
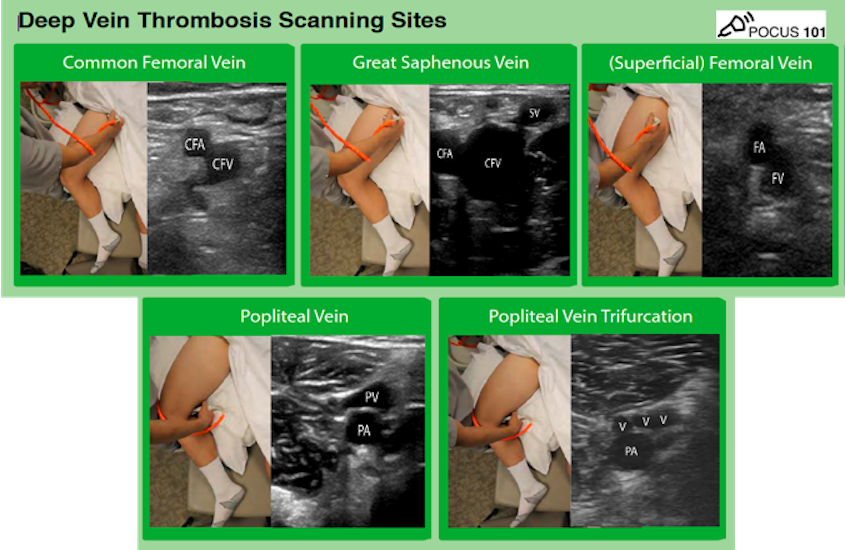
POCUS Assessment for DVT [2-3]
Key Indications
Clinical suspicion for DVT
Unexplained shock/arrest w/ equivocal assessment of right heart strain
Probe selection
High frequency linear array (unless large body habitus warrants lower frequency probe)
Patient positioning
Femoral: externally rotate and flex leg / "frog leg" position (helps to place pillow under the knee for comfort)
Popliteal:
frog leg, or
have patient flex their knee (foot is flat on the bed)
hang their leg over the edge of the bed
prone position
Elevate head of bed to help encourage venous pooling in lower extremities
Technique
Place probe in transverse orientation near the inguinal ligament
Slide probe caudally along the femoral vein, fully compressing every 1-2 cm
Must visualize the following regions at minimum:
Common femoral vein (near level of inguinal ligament)
Greater saphenous vein as it branches off medially/superficially
While the GSV is considered a superficial vein, a clot within 3cm of the SFJ or >5cm in size should be treated as a DVT.
Deep femoral vein as it branches off deep to the femoral vein
Popliteal vein through entire popliteal fossa until it trifurcates into calf veins
Pearls & Pitfalls
Proper positioning — frog leg pt to better expose the femoral vessels; can flex knee or have pt lie supine for popliteal visualization
Make sure the probe is perpendicular to body and directly over the vein to avoid false interpretation
Adequate compression = applying enough pressure so that the adjacent arterial walls start to compress; if a normal vein, the walls should completely touch & the lumen should disappear completely
Once a clot is clearly seen, there’s no need to compress
An acute DVT may be echo-lucent and the only indication will be incompressibility of vein
Can also apply Color Doppler and/or attempt augmentation or respiratory variability with flow, but compression is the best technique
Beware of lymph nodes, superficial thrombophlebitis, abscess, etc. as these can mimic DVT.
What Does the Evidence Show?
Assessing for vein compressibility with ultrasound has high sensitivity & specificity for detecting clinically suspected DVT [4]
Emergency physicians can quickly & accuracy diagnose DVT in the ED [5]. Even EM residents with minimal training can diagnose DVT with fairly good accuracy [6].
POCUS (3-point DVT study) shown to have high sensitivity 93%, specificity 90% compared to radiology-performed DVT study [7]
Venous compression POCUS study by emergency physicians significantly reduced time to disposition compared to radiology-performed studies [8-9]
Take Home Points
In patients with clinical suspicion for DVT, POCUS is a reliable way to quickly assess for DVT & is especially useful if the patient is unstable
Assessment of the femoral and popliteal regions are key
An acute DVT may be echo-lucent and an incompressible vein will be the only clue
False positives can occur with incorrect probe placement, so make sure probe is perpendicular to pt’s body
POCUS findings can expedite diagnosis and treatment
A negative scan may warrant D-dimer or follow up scan
POST BY: DR. ANNA WILLIAMS, PGY1
FACULTY EDITING BY: DR. LAUREN MCCAFFERTY
References
Garrett John, Kline Jeffery. Venous Thromboembolism. In: Mattu A and Swadron S, ed. CorePendium. Burbank, CA: CorePendium, LLC. Updated April 28, 2021. Accessed April 28, 2021
Noble V, Nelson B. Manual of Emergency Medicine and Critical Care Ultrasound, 2nd ed. Cambridge: Cambridge UP, 2011.
Ma OJ, Mateer JR, Reardon RF, & Joing S. (2014). Ma and Mateer's Emergency Ultrasound. New York, NY: McGraw-Hill Education.
Lensing AWA, Prandoni P, Brandjes D, et al.: Detection of deep-vein thrombosis by real-time B-mode ultrasonography. N Engl J Med 320:342–345, 1989.
Blaivas M, Lambert MJ, Harwood RA, et al.: Lower-extremity Doppler for deep venous thrombosis—Can emergency physicians be accurate and fast? Acad Emerg Med 7:120–126, 2000.
Jacoby J, Cesta M, Axelband J, et al.: Can emergency medicine residents detect acute deep venous thrombosis with a limited, two-site ultrasound examination? J EmergMed 32:197–200, 2007.
Pedraza Garcia J, Valle Alonso J, Ceballos Garcia P, et al. Comparison of the accuracy of emergency-department-performed point-of-care ultrasound (POCUS) in the diagnosis of lower extremity deep vein thrombosis. J Emerg Med. 2018; 54( 5): 656–664.
Theodoro D, Blaivas M, Duggal S, et al.: Real-time B- mode ultrasound in the ED saves time in the diagnosis of deep vein thrombosis (DVT). Am J Emerg Med 22:197–200, 2004.
Seyedhosseini J, Fadavi A, Vahidi E, Saeedi M, Momeni M. Impact of point-of-care ultrasound on disposition time of patients presenting with lower extremity deep vein thrombosis, done by emergency physicians. Turkish J Emerg Med. 2018; 18 20-24.