Intern Ultrasound of the Month: Ectopic Pregnancy
- Dr. Haley Durdella, PGY1
The Case
23yo female G2P0010 unknown gestational age presented to the ED for vaginal bleeding. She reported 2 weeks of spotting and took a home pregnancy test, which was positive. Was seen at an outside facility where pregnancy was confirmed via serum test though no imaging performed. She continued to have spotting, along with diffuse abdominal cramping so she came to our ED for another evaluation. ROS otherwise negative. Last normal menses was roughly a little over a month prior to onset of spotting.
Vitals: BP 125/82, HR 100, RR 18, afebrile, SpO2 100% room air
The patient was well-appearing, in no distress. Her abdomen was soft, nondistended, nontender without any signs of peritonitis.
Transabdominal point-of-care ultrasound was performed…
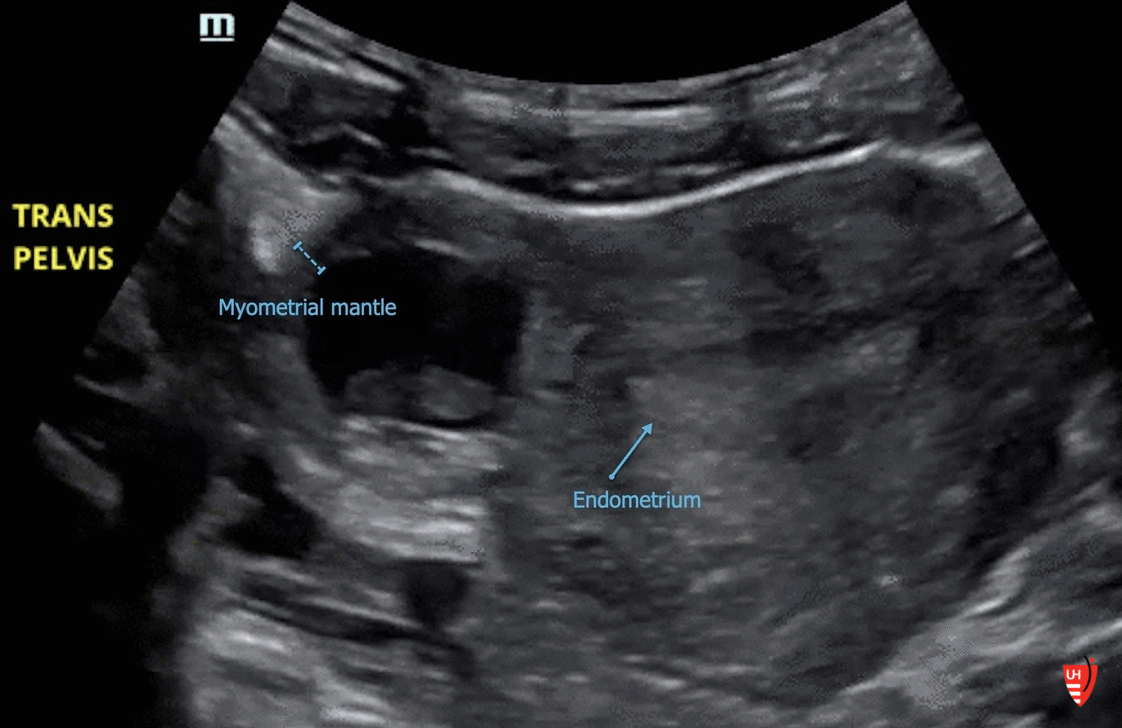
POCUS findings: Thickened endometrium with no IUP present. A live gestational sac was visualized along the right outer edge of the uterus with increased vascularity. Findings concerning for ectopic pregnancy. FAST exam (not shown) was negative.
Clinical course continued: OB was consulted. Given her stability, they requested a “formal” transvaginal ultrasound, which showed a right adnexal/paraovarian ectopic (images below). She was she was taken to the OR where laparoscopy confirmed a right tubal ectopic pregnancy. Salpingectomy performed without complication, and she was discharged directly from the PACU.
Ectopic Pregnancy
Ectopic pregnancy is any gestation implanted outside the endometrial cavity of the uterus
Types seen below. Vast majority in the Fallopian tubes (including this patient’s)
Account for 2-13% of pregnancies
Risk factors include: pelvic inflammatory disease, history of prior ectopic or surgery involving Fallopian tubes
Early Pregnancy Point-of-Care Ultrasound
Technique (transabdominal approach)
Curvilinear probe (linear probe if small enough body habitus)
Sagittal & transverse views (probe marker toward patient’s head and right, respectively).
Fan through entire pelvis for complete assessment
Evaluate for presence of IUP & its location
A full bladder provides a good acoustic window & optimizes exam. If you’re getting a suboptimal view, consider hydrating the patient and repeating scan shortly after (can still save time if you can avoid sending to radiology)
Primary Goal: Rule in IUP
IUP = gestational sac + yolk sac +/- fetal pole… within the endometrial cavity*
Gestational sac alone is NOT an IUP — could be pseudogestational sac (usually small, sometimes irregular, endometrial fluid collection) often seen with ectopic
Double decidual sign (two concentric echogenic rings around a gestational sac) is suggestive of, but NOT confirmatory for, IUP
+IUP essentially rules out ectopic pregnancy (In the absence of fertility treatment)
No IUP = ectopic until proven otherwise
If transabdominal view is nondiagnostic, you need transvaginal study
Findings suggestive of ectopic but nonspecific
Free fluid — perform FAST exam in any patient with suspected ectopic, even if stable
A small amount of fluid (<25 cc) in the pelvis may be physiologic
Free fluid in RUQ (liver tip/inferior pole of the kidney is most sensitive) predicts need for operative intervention
+pregnancy + free fluid = ectopic until proven otherwise
Tubal/adnexal ring — echogenic cystic structure found in the adnexa, tends to have thicker wall than ovarian cysts
Complex adnexal mass — often associated with increased vascularity (“ring of fire”), may or may not see products of conception
*A Potential Pitfall: interstitial ectopic pregnancy
What is it? —> gestation in the interstitial portion of the Fallopian tube (the part closest to the uterus), surrounded only by myometrium.
The rich blood supply of the myometrium allows for larger growth (compared to that of other ectopics) & rupture is associated with profuse, potentially life-threatening, bleeding
Can be easily mistaken for true intrauterine within endometrial cavity, especially on transabdominal ultrasound
—> How to differentiate from true IUP:
Assess location — is the gestation eccentrically located ? i.e. off midline or not within endometrial cavity (note that fibroids or other structural abnormalities may cause this as well)
Measure myometrial mantle thickness — Less than 5-8 mm is concerning for ectopic pregnancy (variable cutoffs but < 5 is definitely highly concerning)
Measure the outer edge of gestational sac to outer edge of uterus at its thinnest location
> 1 cm from gestational sac to most lateral edge of endometrial cavity
Interstitial line sign: fine echogenic line extending from the endometrial stripe to the interstitial gestational sac (diagnostic for this type of pregnancy)
Take Home Points
Obtain sagittal and transverse views and fan through the entire pelvis every time
Goal with POCUS: rule in IUP (GS + YS +/- FP) . If unable to confirm, it’s an ectopic until proven otherwise!
Beware of eccentrically located gestation. Myometrial mantle <5-8mm concerning for ectopic (higher morbidity/mortality with interstitial ectopic)
Perform FAST exam if concerned for ectopic. +RUQ predicts need for OR.
POST BY: DR. HALEY DURDELLA, PGY1
FACULTY EDITING BY: DR. LAUREN MCCAFFERTY
References
Bouyer J, Coste J, Fernandez H, Pouly JL, Job-Spira N. Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Human reproduction. 2002; 17(12):3224-30.
Barnhart KT. Clinical practice. Ectopic pregnancy. N Engl J Med. 2009; 361(4):379-87.
Dawson M, Mallin M. Introduction to Bedside Ultrasound: Vol 1. Lexington, KY: Emergency Ultrasound Solutions, 2013.
Jones R, Goldstein J. Point-of-Care OB Ultrasound, 1st ed. American College of Emergency Physicians, 2016. iBooks.
Ma O, Mateer J et al. Emergency Ultrasound, 3rd ed. McGraw-Hill Education. 2014.
Noble V, Nelson B. Manual of Emergency Medicine and Critical Care Ultrasound, 2nd ed. Cambridge: Cambridge UP, 2011.
Moore C, Todd WM, O’Brien E, Lin H. Free fluid in Morison’s pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007; 14: 755–758