Intern Ultrasound of the Month: Retinal Detachment
The Case
A 45-year-old woman with a past medical history of diabetic neuropathy, hypertension, and migraines presented to the emergency department with one day of left eye blurriness and vision change. The patient also reported a headache with photophobia and phonophobia, similar to past migraines.
Physical exam was notable for visual acuity of 20/200 in the left (affected) eye and 20/40 in the right eye with no pain with extraocular movements and no relative afferent pupillary defect.
Ocular point-of-care ultrasound (POCUS) was performed and showed the following:
POCUS Findings: There is a hyperechoic linear membrane within the vitreous attached posteriorly at the lateral aspect of the optic nerve that does not cross the midline, which indicates a retinal detachment. Additionally, there is a small amount of mobile echogenic matter floating in the posterior chamber, consistent with a vitreous hemorrhage.
How to Do an Ocular POCUS
Equipment Needed:
Ultrasound machine with a high-frequency linear transducer (10-15 MHz)
Gel
Tegaderm
Patient Preparation:
Position the patient comfortably, either lying supine or in a reclined position.
Explain the procedure to the patient to alleviate anxiety.
Apply a tegaderm directly over the closed eye, avoiding air trapping under the plastic film as it can create artifacts that will limit your exam.
Apply a copious amount of gel over the Tegaderm to help ensure the probe does not contact the eye directly and to facilitate sound wave transmission. This also reduces the amount of pressure you need to apply to the eye to get good visualization of structures.
Equipment Preparation:
Ensure the ultrasound machine is set to the appropriate settings for ocular imaging (ocular or superficial preset is best).
Select the high-frequency linear transducer (10-15 MHz).
Scanning Technique:
Rest your hand lightly on the bridge of the patient’s nose or face to stabilize the transducer and control the amount of pressure you apply.
Obtain a transverse view (probe marker pointing toward the patient’s right) with the transducer perpendicular to the eye and fan through the entire eye.
Visualize the following anatomic structures (anterior to posterior): eyelid, anterior chamber, lens, iris, vitreous body, retina, optic nerve
Then, perform a dynamic/kinetic exam by asking your patient to look left and right.
Obtain a sagittal view by rotating the transducer 90 degrees so that the indicator points superiorly (toward patient’s head). Visualize similar structures as you did in the transverse view and ask the patient to look up and down (superior and inferior).
When evaluating the vitreous body for pathology, be sure to increase the gain to help detect subtle intraocular pathology that may be missed with normal gain settings (1).
Figure 1. Eye anatomy (1)
Figure 2. Eye anatomy on ultrasound
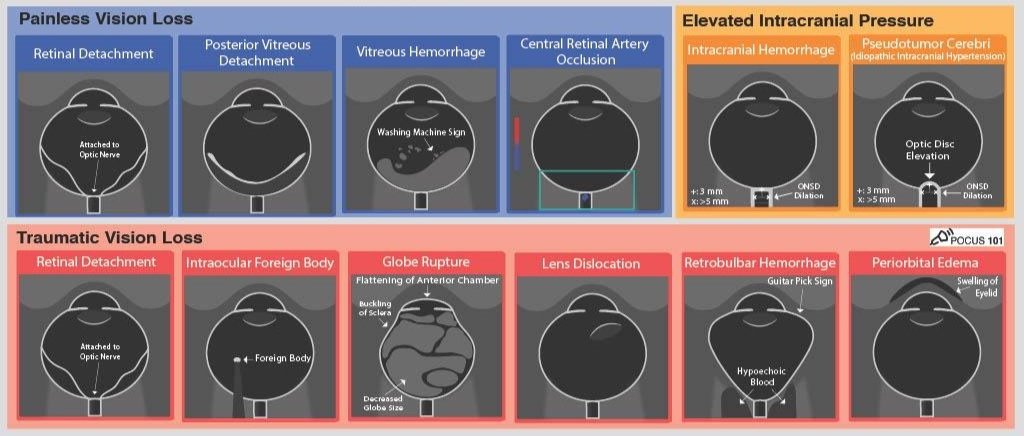
POCUS Indications & Potential Associated Pathology:
Painless Vision Changes/Loss
Retinal and Vitreous Detachment, Vitreous Hemorrhage
Presents as flashers/floaters and may have partial/complete vision loss. See below for more details.
Central Retinal Artery Occlusion
Patient typically have sudden painless monocular vision loss. Ultrasound findings may include a lack of arterial flow of the central retinal artery with color doppler as well as a retrobulbar hyperechoic spot (1,2).
Headache
Increased Intracranial Pressure and Papilledema
Since the optic nerve communicates with the subarachnoid space, an increase in intracranial pressure (ICP) leads to optic nerve sheath expansion as well as optic disc bulging into the vitreous chamber. Studies have shown a correlation between increased ICP and optic nerve sheath diameter (ONSD) greater than 5 mm (measured 3 mm posterior to the retina) or optic disc elevation greater than 6mm. The evidence for ONSD is somewhat poor, and optic disc elevation may be a more promising indicator (3-5).
Trauma
Lens Dislocation
The lens can be seen as a bi-convex hyperechoic structure in the vitreous chamber outside of its normal position behind the iris.
Retrobulbar Hematoma
This is an accumulation of blood in the retrobulbar space that can lead to pain, increased intraocular pressure, ischemia, and ultimately necrosis of the optic nerve and is considered an ocular emergency. The increased retro-bulbar pressure distorts the globe into a cone-like shape.
Periorbital Edema — Consensual pupillary response & extraocular movement
Ultrasound can help visualize consensual pupillary response and extraocular movement when significant periorbital soft tissue swelling prevents an adequate exam (including direct pupillary reflex or extraocular movement) of the affected eye.
Foreign Body
These will appear echogenic (including wood) and can be seen within or around the globe. Metallic objects will often have reverberation artifact. Visualization of a foreign body should raise concern for globe rupture.
Globe Rupture
Ultrasound is NOT recommended if you have a high suspicion of globe rupture. If visualized sonographically, there is usually a loss of the spherical shape of the globe, buckling of the sclera, compression/flattening of the anterior chamber, and may appear as a heterogeneous collection of hematoma, blood, and vitreous humor in the posterior chamber (1-2).
Figure 3. Illustration of ocular pathology detectable on ultrasound (1)
Retinal Detachment
Ocular complaints represent 2-3% of all emergency department visits with 40% being emergent conditions (6-7). A retinal detachment is considered an ocular emergency and requires prompt ophthalmology evaluation. Patients often present with painless vision changes, including flashes, floaters, or a curtain coming down over their eye. In addition to a fundoscopic exam, retinal detachments can be diagnosed with ultrasound. In a meta-analysis study, detection of a retinal detachment on POCUS performed by emergency physicians had both a sensitivity and specificity of 94% (8).
Sonographic findings:
Retinal Separation — Ultrasound can detect the separation of the neurosensory retina from the retinal pigment epithelium. This separation is often seen as a hypoechoic space between the two layers with the detached retina within the vitreous body.
Echogenicity/key features — The detached retina typically appears as a thick hyperechoic undulating membrane that is tethered posteriorly to the optic nerve and may be saddle-shaped or V-shaped. Its attachment points are on the same side of the globe and the membrane generally does not cross midline. It has a snake-like movement with a kinetic exam and tends to be less mobile than vitreous detachment/hemorrhage.
Retinal tear — A retinal tear or break may be visualized as a focal discontinuity in the retina on ultrasound, though this is often not well-visualized.
Location and extent — Ultrasound can help determine the location and extent of the detachment, which is crucial for surgical planning. It may helpful in distinguishing the type of detachment, i.e. rhegmatogenous (caused by retinal tears) vs non-rhegmatogenous (caused by other factors), but simply identifying the retinal detachment, not the type, is not the focus of ocular ultrasound (1).
Vitreous Hemorrhage
While this is not considered an ocular emergency, vitreous hemorrhage can also be readily detected with POCUS. In a study by Propst et al, POCUS performed by emergency physicians had a sensitivity and specificity of 81.9% and 82.3%, respectively (9).
Figure 4a. Retinal detachment - note its posterior relation to the optic nerve
Figure 4b. Retinal detachment - dynamic exam.
Figure 5. Vitreous hemorrhage
Sonographic findings:
Echogenicity/key features — Vitreous hemorrhage may appear as dense, variably echogenic material within the vitreous body that is often best seen with increased gain. It is generally highly mobile and readily swirls with dynamic movement, giving it a ‘washing machine’ appearance.
Location — The blood may be dispersed throughout the vitreous chamber but often layers in the more posterior, dependent portion.
*A potential mimicker of vitreous hemorrhage is asteroid hyalosis, which is reviewed in this previous blog post by Dr. Eni Gros (10).
Figure 6. Vitreous detachment
Vitreous Detachment
A posterior vitreous detachment (PVD) often presents with similar symptoms as a retinal detachment but is not considered an ocular emergency.
Sonographic findings: Thinner hyperechoic membrane that is NOT tethered to the optic nerve. It often crosses midline and moves more freely compared to a retinal detachment, giving it a ‘swaying seaweed’ appearance (1-2).
Case Conclusion
Ophthalmology concluded that the patient had a tractional retinal detachment (i.e. separation due to tractional forces) without breaks, as well as dense vitreous hemorrhage. The patient underwent a pars plana vitrectomy, membrane peel, and endolaser. Post-operatively, optical coherence tomography (below) showed with an intact retina and no detachment seen.
Take Home Points
POCUS has good diagnostic utility for several ocular pathologies, including retinal detachment, which is an ocular emergency, as well as vitreous detachment/hemorrhage, among others.
A retinal detachment appears as a thick echogenic membranes within the vitreous that attaches posteriorly at/near the optic nerve, does not cross midline, and has a serpentine-like motion with a dynamic exam. In contrast, a posterior vitreous detachment or vitreous hemorrhage have no relation to the optic nerve, can cross midline, and are more mobile or free floating.
Have a systemic approach to ocular ultrasound, making sure you visualize anatomic structures, increase gain when evaluating within the vitreous body, and perform a dynamic exam.
AUTHORED BY: YANINA GUEVARA, MD
FACULTY CO-AUTHOR/EDITOR: LAUREN MCCAFFERTY, MD
References
Ahn, Jessica. “Ocular Ultrasound Made Easy: Step-By-Step Guide.” POCUS 101. September 5th, 2023. https://www.pocus101.com/ocular-ultrasound-made-easy-step-by-step-guide/
Bates A, Goett HJ. Ocular Ultrasound. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459120/
Ohle R, McIsaac SM, Woo MY, Perry JJ. Sonography of the Optic Nerve Sheath Diameter for Detection of Raised Intracranial Pressure Compared to Computed Tomography: A Systematic Review and Meta-analysis. J Ultrasound Med. 2015 Jul;34(7):1285-94.
Agrawal D, Raghavendran K, Zhao L, Rajajee V. A Prospective Study of Optic Nerve Ultrasound for the Detection of Elevated Intracranial Pressure in Severe Traumatic Brain Injury. Crit Care Med. 2020 Dec;48(12):e1278-e1285.
Teismann N, Lenaghan P, Nolan R, Stein J, Green A. Point-of-care ocular ultrasound to detect optic disc swelling. Acad Emerg Med. 2013 Sep;20(9):920-5.
Walker RA, Adhikari S. Eye emergencies. In: Tintinalli JE, Stapczynski S, Ma OJ, Yealy DM, Meckler JD, Cline DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Chicago, IL: McGraw-Hill Medical; 2011: 236:1517-1549.
Channa R, Zafar SN, Canner JK, Haring RS, Schneider EB, Friedman DS. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016; 134(3):312-319.
Propst SL, Kirschner JM, Strachan CC, Roumpf SK, Menard LM, Sarmiento EJ, Hunter BR. Ocular Point-of-Care Ultrasonography to Diagnose Posterior Chamber Abnormalities: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020; 3(2):e1921460.
Lahham S, Shniter I, Thompson M, et al. Point-of-Care Ultrasonography in the Diagnosis of Retinal Detachment, Vitreous Hemorrhage, and Vitreous Detachment in the Emergency Department. JAMA Netw Open. 2019; 2(4):e192162.
Gros E, McCafferty L. A Mimicker of Vitreous Hemorrhage: Asteriod Hyalosis. The Land of EM POCUS Blog. April 11, 2022. Accessed September 5th, 2023.